Complications from Breast Enlargement Surgery are rare. By far most patients that undergo this procedure experience a very safe recovery and enjoy a beautiful long-term result without problems as the satisfaction rate of this procedure is one of the highest among plastic surgery procedures. However, complications can occur and the following is a list of local complications and adverse outcomes from the official FDA website (United States Food & Drug Administration) which is the regulatory authority for breast implants in the United States. Most of the complications listed below happen at a rate smaller than 1% with the most frequent being capsular contracture which happens at a rate of approximately 4-5%. The complications are listed alphabetically, not in order of how often they occur and most of complications listed are issues that patients almost never experience.
Implant Complications, FDA official information (update June 16, 2020)
Asymmetry
The breasts are uneven in appearance in terms of size, shape or breast level.
Breast Pain
Pain in the nipple or breast area.
Breast Tissue Atrophy
Thinning and shrinking of the skin.
Calcification/Calcium Deposits
Hard lumps under the skin around the implant. These can be mistaken for cancer during mammography, resulting in additional surgery.
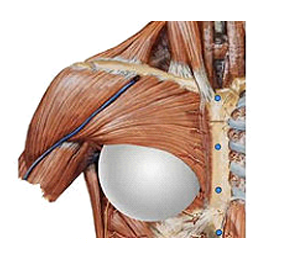
Capsular Contracture
Tightening of the tissue capsule around an implant, resulting in firmness or hardening of the breast and squeezing of the implant if severe.
Chest Wall Deformity
Chest wall or underlying rib cage appears deformed.
Deflation
Leakage of the saltwater (saline) solution from a saline-filled breast implant, often due to a valve leak or a tear or cut in the implant shell (rupture), with partial or complete collapse of the implant.
Delayed Wound Healing
Incision site fails to heal normally or takes longer to heal.
Extrusion
The skin breaks down and the implant appears through the skin.
Hematoma
Collection of blood near the surgical site. May cause swelling, bruising and pain. Hematomas usually occur soon after surgery, but can occur any time there is injury to the breast. The body may absorb small hematomas, but large ones may require medical intervention, such as surgical draining.
Iatrogenic Injury/Damage
Injury or damage to tissue or implant as a result of implant surgery.
Infection, including Toxic Shock Syndrome
Occurs when wounds are contaminated with microorganisms, such as bacteria or fungi. Most infections resulting from surgery appear within a few days to a week, but infection is possible any time after surgery. If an infection does not respond to antibiotics, the implant may need to be removed.
Inflammation/Irritation
Response by the body to an infection or injury. Demonstrated by redness, swelling, warmth, pain and or/loss of function.
Lymphedema or Lymphadenopathy
Swollen or enlarged lymph nodes
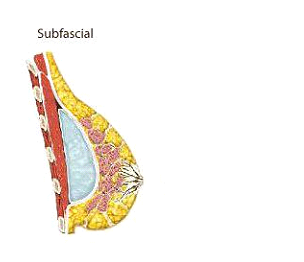
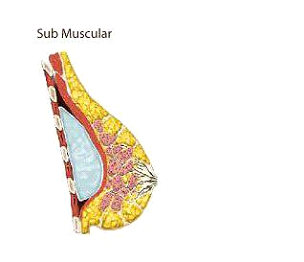
Malposition/Displacement
The implant is not in the correct position in the breast. This can happen during surgery or afterwards if the implant moves or shifts from its original location. Shifting can be caused by factors such as gravity, trauma or capsular contracture.
Necrosis
Dead skin or tissue around the breast. Necrosis can be caused by infection, use of steroids in the surgical breast pocket, smoking, chemotherapy/radiation, and excessive heat or cold therapy.
Nipple/Breast Sensation Changes
An increase or decrease in the feeling in the nipple and/or breast. Can vary in degree and may be temporary or permanent. May affect sexual response or breast feeding.
Palpability
The implant can be felt through the skin.
Ptosis
Breast sagging that is usually the result of normal aging, pregnancy or weight loss.
Redness/Bruising
Bleeding at the time of surgery can cause the skin to change color. This is an expected symptom due to surgery, and is likely temporary.
Rupture
A tear or hole in the implant’s outer shell.
Seroma
Collection of fluid around the implant. May cause swelling, pain and bruising. The body may absorb small seromas. Large ones will require a surgical drain.
Skin Rash
A rash on or around the breast.
Unsatisfactory Style/Size
Patient or doctor is not satisfied with the overall look based on the style or size of the implant used.
Visibility
The implant can be seen through the skin.
Wrinkling/Rippling
Wrinkling of the implant that can be felt or seen through the skin.
Link: https://www.fda.gov/medical-devices/breast-implants/risks-and-complications-breast-implants